Which Of The Following Hormones Controls The Release Of Anterior Pituitary Gonadotropins
Chapter 24. Fauna Reproduction and Development
24.iv. Hormonal Control of Homo Reproduction
Learning Objectives
Past the terminate of this chapter, you will exist able to:
- Depict the roles of male person and female reproductive hormones
- Discuss the interplay of the ovarian and menstrual cycles
- Draw the process of menopause
The human being male and female reproductive cycles are controlled past the interaction of hormones from the hypothalamus and anterior pituitary with hormones from reproductive tissues and organs. In both sexes, the hypothalamus monitors and causes the release of hormones from the pituitary gland. When the reproductive hormone is required, the hypothalamus sends a gonadotropin-releasing hormone (GnRH) to the anterior pituitary. This causes the release of follicle stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary into the blood. Note that the trunk must accomplish puberty in guild for the adrenals to release the hormones that must be nowadays for GnRH to be produced. Although FSH and LH are named after their functions in female reproduction, they are produced in both sexes and play of import roles in controlling reproduction. Other hormones have specific functions in the male and female reproductive systems.
Male Hormones
At the onset of puberty, the hypothalamus causes the release of FSH and LH into the male system for the first time. FSH enters the testes and stimulates the Sertoli cells to begin facilitating spermatogenesis using negative feedback, every bit illustrated in
Effigy 24.14. LH besides enters the testes and stimulates the interstitial cells of Leydig to brand and release testosterone into the testes and the blood.
Testosterone, the hormone responsible for the secondary sexual characteristics that develop in the male person during boyhood, stimulates spermatogenesis. These secondary sex characteristics include a deepening of the phonation, the growth of facial, axillary, and pubic pilus, and the beginnings of the sexual activity drive.
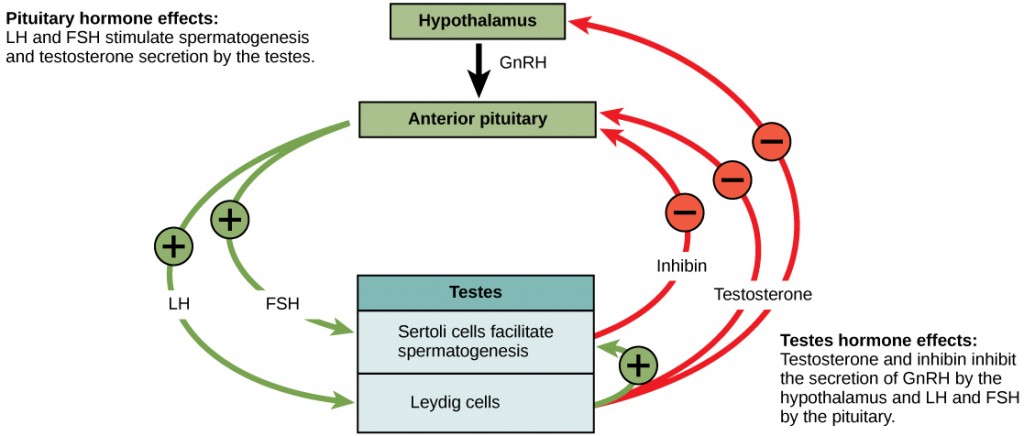
A negative feedback system occurs in the male with rise levels of testosterone interim on the hypothalamus and anterior pituitary to inhibit the release of GnRH, FSH, and LH. The Sertoli cells produce the hormone inhibin, which is released into the blood when the sperm count is also high. This inhibits the release of GnRH and FSH, which will cause spermatogenesis to deadening downward. If the sperm count reaches twenty million/ml, the Sertoli cells cease the release of inhibin, and the sperm count increases.
Female Hormones
The command of reproduction in females is more complex. Every bit with the male person, the anterior pituitary hormones cause the release of the hormones FSH and LH. In addition, estrogens and progesterone are released from the developing follicles. Estrogen is the reproductive hormone in females that assists in endometrial regrowth, ovulation, and calcium absorption; it is also responsible for the secondary sexual characteristics of females. These include chest evolution, flaring of the hips, and a shorter period necessary for bone maturation. Progesterone assists in endometrial re-growth and inhibition of FSH and LH release.
In females, FSH stimulates development of egg cells, called ova, which develop in structures called follicles. Follicle cells produce the hormone inhibin, which inhibits FSH production. LH likewise plays a role in the development of ova, induction of ovulation, and stimulation of estradiol and progesterone production by the ovaries. Estradiol and progesterone are steroid hormones that ready the body for pregnancy. Estradiol produces secondary sex characteristics in females, while both estradiol and progesterone regulate the menstrual cycle.
The Ovarian Cycle and the Menstrual Cycle
The ovarian cycle governs the preparation of endocrine tissues and release of eggs, while the menstrual wheel governs the grooming and maintenance of the uterine lining. These cycles occur concurrently and are coordinated over a 22–32 twenty-four hour period cycle, with an average length of 28 days.
The first one-half of the ovarian bike is the follicular phase shown in Figure 24.15. Slowly rising levels of FSH and LH cause the growth of follicles on the surface of the ovary. This process prepares the egg for ovulation. As the follicles grow, they brainstorm releasing estrogens and a low level of progesterone. Progesterone maintains the endometrium to help ensure pregnancy. The trip through the fallopian tube takes about seven days. At this stage of development, chosen the morula, in that location are xxx-sixty cells. If pregnancy implantation does not occur, the lining is sloughed off. Later about five days, estrogen levels ascent and the menstrual bike enters the proliferative stage. The endometrium begins to regrow, replacing the blood vessels and glands that deteriorated during the finish of the last cycle.
Which of the following statements about hormone regulation of the female person reproductive bike is false?
- LH and FSH are produced in the pituitary, and estradiol and progesterone are produced in the ovaries.
- Estradiol and progesterone secreted from the corpus luteum cause the endometrium to thicken.
- Both progesterone and estradiol are produced by the follicles.
- Secretion of GnRH by the hypothalamus is inhibited by low levels of estradiol only stimulated by high levels of estradiol.
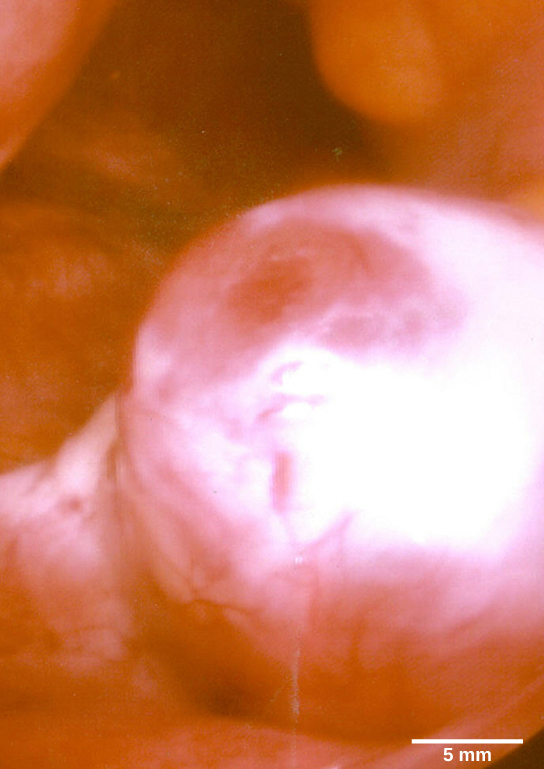
Just prior to the centre of the cycle (approximately mean solar day 14), the high level of estrogen causes FSH and especially LH to rise rapidly, so fall. The spike in LH causes ovulation: the almost mature follicle, like that shown in Figure 24.16, ruptures and releases its egg. The follicles that did non rupture degenerate and their eggs are lost. The level of estrogen decreases when the extra follicles degenerate.
Post-obit ovulation, the ovarian cycle enters its luteal phase, illustrated in Figure 24.15 and the menstrual cycle enters its secretory stage, both of which run from almost day 15 to 28. The luteal and secretory phases refer to changes in the ruptured follicle. The cells in the follicle undergo physical changes and produce a construction chosen a corpus luteum. The corpus luteum produces estrogen and progesterone. The progesterone facilitates the regrowth of the uterine lining and inhibits the release of further FSH and LH. The uterus is beingness prepared to accept a fertilized egg, should it occur during this cycle. The inhibition of FSH and LH prevents whatsoever further eggs and follicles from developing, while the progesterone is elevated. The level of estrogen produced by the corpus luteum increases to a steady level for the adjacent few days.
If no fertilized egg is implanted into the uterus, the corpus luteum degenerates and the levels of estrogen and progesterone decrease. The endometrium begins to degenerate as the progesterone levels drop, initiating the adjacent menstrual cycle. The decrease in progesterone also allows the hypothalamus to send GnRH to the anterior pituitary, releasing FSH and LH and starting the cycles over again. Effigy 24.17 visually compares the ovarian and uterine cycles also as the commensurate hormone levels.
Which of the post-obit statements about the menstrual cycle is false?
- Progesterone levels rise during the luteal phase of the ovarian bike and the secretory phase of the uterine cycle.
- Menstruation occurs only subsequently LH and FSH levels peak.
- Menstruation occurs afterwards progesterone levels drop.
- Estrogen levels rise earlier ovulation, while progesterone levels rise later.
Menopause
As women approach their mid-40s to mid-50s, their ovaries begin to lose their sensitivity to FSH and LH. Menstrual periods get less frequent and finally end; this is menopause. There are even so eggs and potential follicles on the ovaries, just without the stimulation of FSH and LH, they will not produce a viable egg to exist released. The consequence of this is the disability to have children.
The side effects of menopause include hot flashes, heavy sweating (especially at night), headaches, some hair loss, muscle pain, vaginal dryness, insomnia, depression, weight gain, and mood swings. Estrogen is involved in calcium metabolism and, without it, blood levels of calcium decrease. To furnish the blood, calcium is lost from os which may subtract the bone density and atomic number 82 to osteoporosis. Supplementation of estrogen in the class of hormone replacement therapy (HRT) tin prevent bone loss, but the therapy can have negative side effects. While HRT is thought to give some protection from colon cancer, osteoporosis, heart affliction, macular degeneration, and peradventure depression, its negative side furnishings include increased risk of: stroke or heart attack, blood clots, breast cancer, ovarian cancer, endometrial cancer, gall bladder disease, and possibly dementia.
Reproductive Endocrinologist
A reproductive endocrinologist is a physician who treats a multifariousness of hormonal disorders related to reproduction and infertility in both men and women. The disorders include menstrual issues, infertility, pregnancy loss, sexual dysfunction, and menopause. Doctors may use fertility drugs, surgery, or assisted reproductive techniques (ART) in their therapy. Art involves the use of procedures to dispense the egg or sperm to facilitate reproduction, such as in vitro fertilization.
Reproductive endocrinologists undergo all-encompassing medical grooming, commencement in a iv-year residency in obstetrics and gynecology, then in a iii-year fellowship in reproductive endocrinology. To be lath certified in this area, the dr. must pass written and oral exams in both areas.
Summary
The male and female reproductive cycles are controlled by hormones released from the hypothalamus and anterior pituitary besides every bit hormones from reproductive tissues and organs. The hypothalamus monitors the need for the FSH and LH hormones made and released from the anterior pituitary. FSH and LH impact reproductive structures to crusade the formation of sperm and the preparation of eggs for release and possible fertilization. In the male, FSH and LH stimulate Sertoli cells and interstitial cells of Leydig in the testes to facilitate sperm product. The Leydig cells produce testosterone, which also is responsible for the secondary sexual characteristics of males. In females, FSH and LH cause estrogen and progesterone to be produced. They regulate the female reproductive system which is divided into the ovarian bicycle and the menstrual wheel. Menopause occurs when the ovaries lose their sensitivity to FSH and LH and the female person reproductive cycles tedious to a stop.
Exercises
- Which of the post-obit statements about hormone regulation of the female reproductive cycle is simulated?
- LH and FSH are produced in the pituitary, and estradiol and progesterone are produced in the ovaries.
- Estradiol and progesterone secreted from the corpus luteum crusade the endometrium to thicken.
- Both progesterone and estradiol are produced by the follicles.
- Secretion of GnRH past the hypothalamus is inhibited by depression levels of estradiol simply stimulated by high levels of estradiol.
- Which of the following statements about the menstrual wheel is imitation?
- Progesterone levels rise during the luteal phase of the ovarian cycle and the secretory phase of the uterine cycle.
- Menstruation occurs only after LH and FSH levels peak.
- Menstruation occurs after progesterone levels drop.
- Estrogen levels rise before ovulation, while progesterone levels rise after.
- Which hormone causes Leydig cells to brand testosterone?
- FSH
- LH
- inhibin
- estrogen
- Which hormone causes FSH and LH to be released?
- testosterone
- estrogen
- GnRH
- progesterone
- Which hormone signals ovulation?
- FSH
- LH
- inhibin
- estrogen
- Which hormone causes the re-growth of the endometrial lining of the uterus?
- testosterone
- estrogen
- GnRH
- progesterone
- If male reproductive pathways are not cyclical, how are they controlled?
- Draw the events in the ovarian cycle leading upwards to ovulation.
Answers
- C
- B
- A
- C
- B
- D
- Negative feedback in the male person organisation is supplied through two hormones: inhibin and testosterone. Inhibin is produced by Sertoli cells when the sperm count exceeds prepare limits. The hormone inhibits GnRH and FSH, decreasing the activity of the Sertoli cells. Increased levels of testosterone impact the release of both GnRH and LH, decreasing the activity of the Leydig cells, resulting in decreased testosterone and sperm production.
- Depression levels of progesterone permit the hypothalamus to send GnRH to the anterior pituitary and cause the release of FSH and LH. FSH stimulates follicles on the ovary to grow and prepare the eggs for ovulation. As the follicles increment in size, they begin to release estrogen and a low level of progesterone into the blood. The level of estrogen rises to a top, causing a spike in the concentration of LH. This causes the most mature follicle to rupture and ovulation occurs.
Glossary
estrogen
reproductive hormone in females that assists in endometrial regrowth, ovulation, and calcium assimilation
follicle stimulating hormone (FSH)
reproductive hormone that causes sperm production in men and follicle development in women
gonadotropin-releasing hormone (GnRH)
hormone from the hypothalamus that causes the release of FSH and LH from the anterior pituitary
inhibin
hormone fabricated by Sertoli cells; provides negative feedback to hypothalamus in control of FSH and GnRH release
interstitial
cell of Leydigcell in seminiferous tubules that makes testosterone
luteinizing hormone (LH)
reproductive hormone in both men and women, causes testosterone product in men and ovulation and lactation in women
menopause
loss of reproductive capacity in women due to decreased sensitivity of the ovaries to FSH and LH
menstrual cycle
bike of the deposition and re-growth of the endometrium
ovarian cycle
cycle of preparation of egg for ovulation and the conversion of the follicle to the corpus luteum
ovulation
release of the egg by the virtually mature follicle
progesterone
reproductive hormone in women; assists in endometrial re-growth and inhibition of FSH and LH release
Sertoli cell
jail cell in seminiferous tubules that assists developing sperm and makes inhibin
testosterone
reproductive hormone in men that assists in sperm production and promoting secondary sexual characteristics
Which Of The Following Hormones Controls The Release Of Anterior Pituitary Gonadotropins,
Source: https://opentextbc.ca/biology/chapter/24-4-hormonal-control-of-human-reproduction/
Posted by: tarverfrose1966.blogspot.com


0 Response to "Which Of The Following Hormones Controls The Release Of Anterior Pituitary Gonadotropins"
Post a Comment